Got Dehydrated Skin?
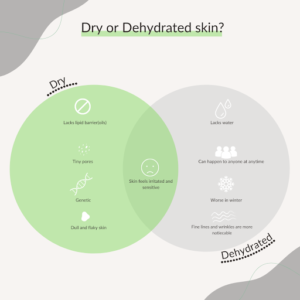
This time of the year brings; falling leaves, cold weather, family gatherings, and compromised skin. Have you noticed that no matter how much lotion you’re
OUR LOCATIONS
SKIN TIGHTENING
SKIN CANCER
SKIN RESURFACING
VASCULAR CORRECTIVE
SPIDER VEIN REMOVAL
MEDICAL AESTHETICANS
PATIENT RESOURCES
OUR LOCATIONS
SKIN TIGHTENING
SKIN CANCER
SKIN RESURFACING
VASCULAR CORRECTIVE
SPIDER VEIN REMOVAL
MEDICAL AESTHETICANS
PATIENT RESOURCES
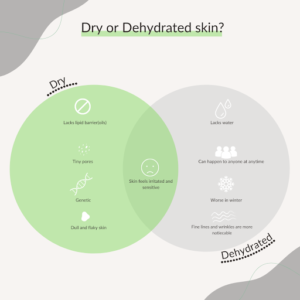
This time of the year brings; falling leaves, cold weather, family gatherings, and compromised skin. Have you noticed that no matter how much lotion you’re
It’s easy to become confused about the different roles and benefits of cosmetic injectables. Botox and dermal fillers such as Juvederm, Restylane and Perlane are
In this age of the selfie, patients are asking for ways to improve their appearance when unflattering photos make them feel self-conscious. Often, the presence
The weather is warmer and the days are longer. Even though the sun feels good on your face, there are various steps you need to
Microneedling is a non-invasive treatment that helps stimulate the production of collagen in the skin, resulting in smoother, firmer, younger-looking skin. New radiofrequency technology takes
The new HydraFacial is not just any facial. Utilizing the latest advances in patented skincare technology, the HydraFacial consists of a three-step process to give
Spider veins are unsightly red, blue or purple veins that get their name from their cluster appearance on the face and the lower extremities. Heredity,
HydraFacial uses patented technology to cleanse, extract, and hydrate skin while infusing highly-effective serums tailored to your specific skin needs. This unique process helps improve
Smiling, laughing and frowning – over time, these repeated expressions lead to expression lines, folds and wrinkles on our faces. There are few treatments more
Whether staying inside to enjoy a roaring fire or going outside into the cold, you can’t escape the effects of the winter air on your
All those holiday parties and gatherings with family and friends are just around the corner, so now is glow time to get your skin looking